The NURSING WIT AND WISDOM project is proud and honored to have been nominated for the 2015 Nightingale Awards!
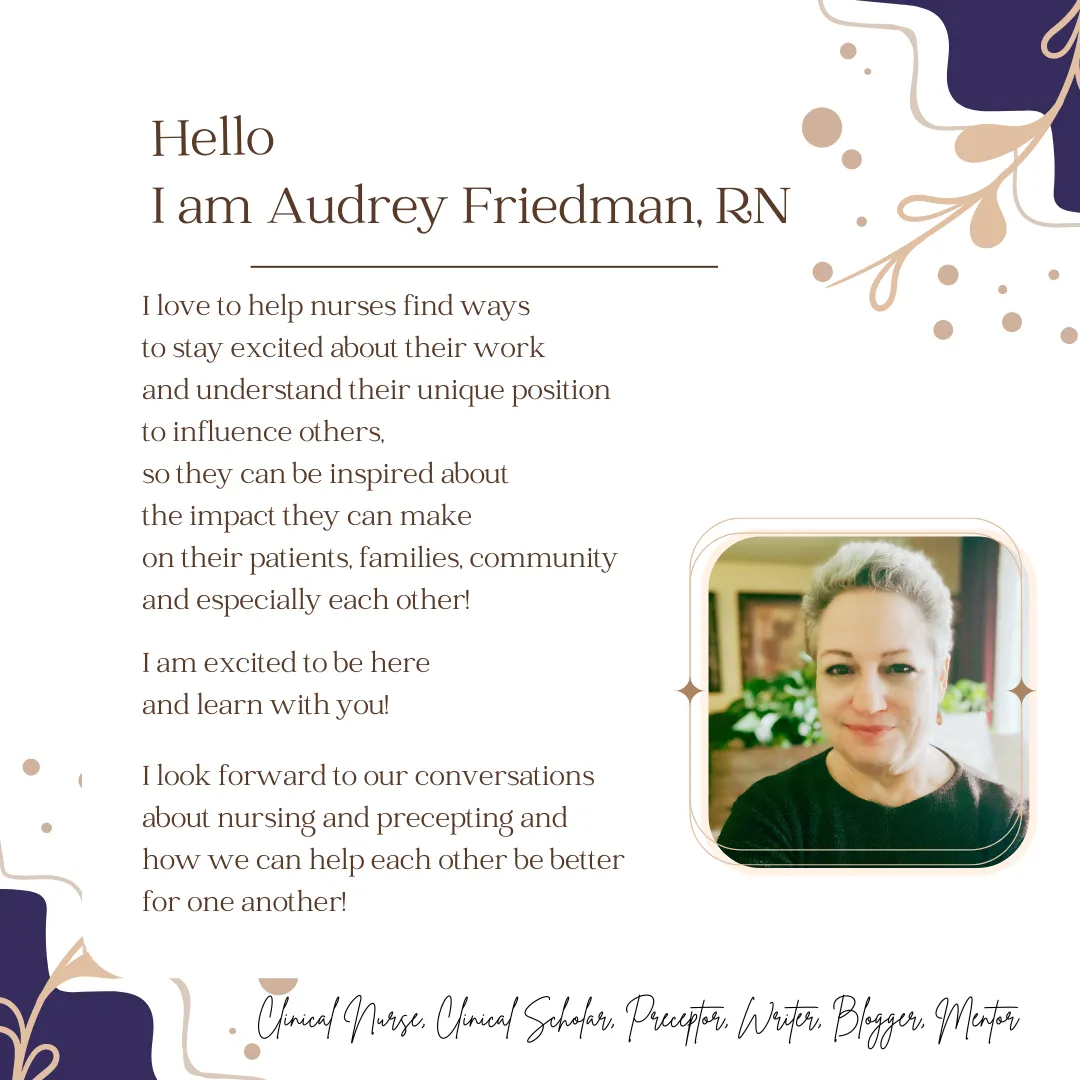
Online Courses for Nurses and Preceptors
Fun ways to learn with Clinical Challenges
Blog with lots of Freebies!
Lots of ways to Inspire and Be Inspired!
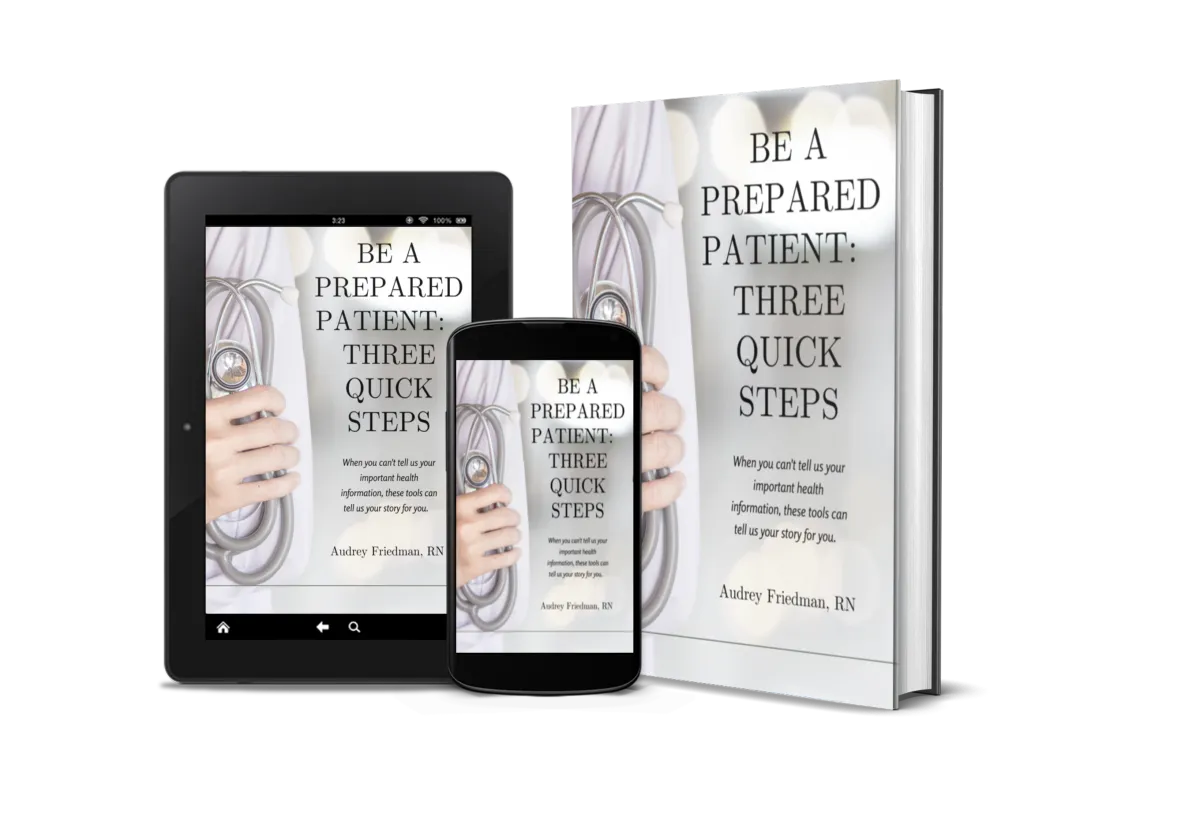
Get Your Free 'Be A Prepared Patient' Kit!
As a nurse who has seen many patients and families come into the hospital and are too sick or unable to tell us their health information, such as diagnoses, treatments and especially devices and medications, I encourage you to DOWNLOAD my FREE PDF BOOKLET with wallet and refrigerator health information cards, so that THE CARDS CAN TELL HEALTHCARE PROVIDERS YOUR STORY IF YOU ARE NOT ABLE TO.
Read my free blog posts
I share nursing stories, resources, tips and tricks for nurses, nurse preceptors and students. And lots of FREE downloads!
Free Courses!
Get started with a FREE COURSE
*Be A Prepared Patient
Courses for nurses, preceptors and students
My courses are designed for nurses and nurse preceptors of all levels who are excited about adding new information, perspectives and skills to their clinical expertise.
Book a coaching call with Audrey RN
I would look forward to helping you on a special project, mentoring you on nursing clinical questions, preceptor skills or staying inspired about nursing!
Read my free blog posts
I share nursing stories, resources, tips and tricks for nurses and nurse preceptors and preceptors. And lots of FREE downloads!
Join my courses for nurses and preceptors
My courses are designed for nurses and nurse preceptors of all levels who are excited about adding new information, perspectives and skills to their clinical expertise.
Free Courses
Get started with a FREE COURSE
*Be A Prepared Patient
Book a coaching call with Audrey
I would look forward to helping you on a special project, mentoring you on nursing clinical, preceptor skills or staying inspired about nurisng!
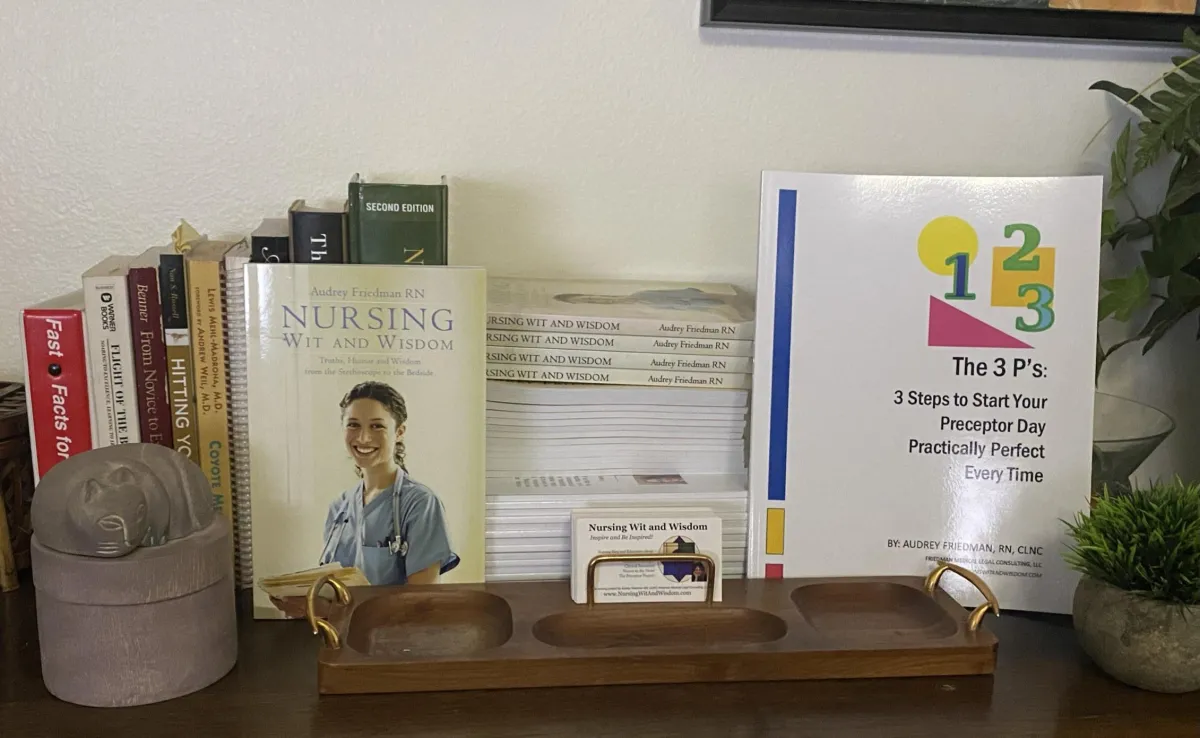
Nurses have the unique privilege to have a backstage pass to our patients' and families' journeys. In the process, we teach, listen, clean up things only your mother or a toxic waste company would touch, and love to wake up doctors in the middle of the night.
And hopefully, we inspire and share our wisdom along the way.
The journey is not only for them, but for us as well. Our own journey as nurses has been seeded by what we experience. Do you see them as gifts or challenges? Can both inspire you?
I hope so!
This is the perfect companion for nurses, nursing students, medical students and all those who share in a nurse's life.
Share it with someone!
Inspire and Be Inspired!
Audrey Friedman, RN
2015 Nightingale Award nominee
"This book should be in the hands of every single nurse on the planet!"
- Sara Davenport

"I have had the pleasure to read quite a few of Audrey's work, and they have always been enjoyable, as well as educational. Don't miss out on a chance to read such a witty, informative, educational and memorable journey with insight only a dedicated nurse could share with us."
Jill Oldehoff

A truly vital and unique perspective!
"Audrey is a woman of exceptional integrity and expertise. She has a depth of experience in the medical field that encompasses both traditional and complimentary therapy knowledge. This gives her the ability to offer a balanced perspective in the industry that is truly vital and unique."
Sara Davenport

An innovative, creative approach to mentoring!
"Audrey has a talent (and uses it) for facilitating other’s efforts to find ways to excel – and earn more, potentially. I am a benefactor of this special ability and recommend her most strongly for her innovative, creative approach to mentoring professional practices."
John Riddell, RN, BS, LNC, Excellence Medical Legal Research & Consulting